There are several different types of blood. Contained within them are different types of cells and countless molecules that give our bodies the needed nutrients to work effectively. The two main types of cells within the blood are red and white blood cells. Red blood cells make up nearly 45% of your blood volume. White blood cells make up less than 1%. What is left over is known as blood plasma, which makes up approximately 55% of your blood volume.
There are several different types of blood. Contained within them are different types of cells and countless molecules that give our bodies the needed nutrients to work effectively. The two main types of cells within the blood are red and white blood cells. Red blood cells make up nearly 45% of your blood volume. White blood cells make up less than 1%. What is left over is known as blood plasma, which makes up approximately 55% of your blood volume.
As to blood types, what type you are will usually depend on the types of blood your parents have, though there can be exceptions like if you receive a bone marrow transplant from someone with a different blood type, your blood type will eventually change, among some caveats like that.
As to why there are different blood types, this isn’t fully understood, though it’s been observed that different blood types play a role in your susceptibility, or lack thereof, to certain diseases and conditions. For example, malaria seems to have been a major contributor to type O being a major thing in places like Africa where about 51% of the populace have type O blood. As to why, it turns out for various reasons type-O blood will generally mean you won’t get as sick if you get malaria.
So what are all the blood types and what’s with the whole positive and negative thing?
There are 8 main types of blood separated into 4 groups, with over 90% of people falling into one of these main groups. The groups are A, B, AB, and O. If you’re now wondering why O and not, for example, “C” to make it A B C, it turns out it originally was called “C” but was later changed to the letter “O” in some regions or the number 0 in others, in both cases to signify zero or null, for reasons we’ll get into.
In any event, these blood types are grouped together by the presence or absence of what is known as an antigen. Antigens are substances within the blood that cause our immune systems to create antibodies- essentially used to recognize invaders. These created antibodies then send anything the immune system thinks is a threat to sleep with fishes.
The specific antigens that create the different blood types are found on the surface of red blood cells and are known as type A and type B. They’re further separated by the presence of another type of antigen known as rH factor. If you have this rH antigen present, you’re considered positive, if not, you’re considered a negative-nancy and nobody likes you- we’re looking at you, Jimmy.
Someone that has type A antigens and rH factor is considered to have type A+ blood. If you have both types of antigens and no rH factor, you have type AB- blood. If you have no A or B antigens then you are type O blood, hence the whole “zero” or “null” thing mentioned before.
All of this matters because of those antibodies your immune system creates. Someone with type A blood will at some point in their earliest months or years for trigger reasons not wholly understood develop antibodies for type B, and someone with type B will have antibodies for type A. Type O has antibodies for both A and B.
This brings us around to why mixing and matching certain, but not all, blood types in a person is a very bad idea. In a nutshell, if you were to give type B blood to someone who is type A, their antibodies for type A would attack the type A red blood cells causing unwanted side effects, including in the extreme various things like kidney failure as your kidneys try to filter out all the destroyed red blood cells. And, of course, regardless of this sort of thing, as you kind of need sufficient blood to keep living, if your immune system destroys a high enough percentage of what you currently have in your body, you’re going to have trouble continuing to be just for that reason, let alone the other complications.
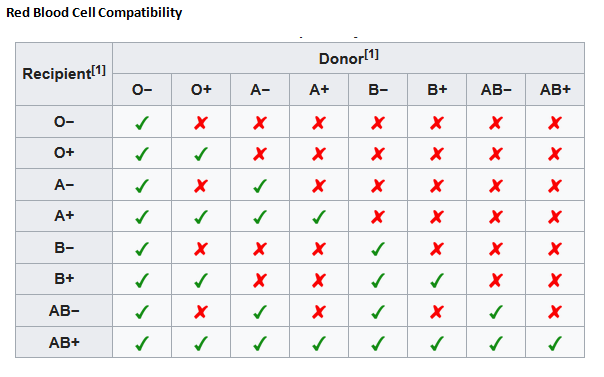
But it’s not always a bad thing to mix and match. For example, disregarding a bit of a caveat about atypical antibodies and the like, someone with type AB+ can actually receive blood from every other main blood type. As to why, if you’ve been following along, this is because these individuals are characterized by having BOTH A and B antigens on their red blood cells, and thus cannot have either antibody in their plasma.
For this reason, those with AB+ blood type are sometimes referred to as universal recipients because they can accept blood from anyone (again, with the caveat about those atypical antibodies). However, the downside of this is that because of the presence of BOTH antigens on type AB red blood cells, people with AB+ blood can only donate blood to others with the same type, and AB- are only able to donate to AB+ or AB- individuals, but able to receive from any of the negative blood types, again with the aforementioned caveats which we’re going to stop saying, but just realize that’s a thing because the universe hates simplicity.
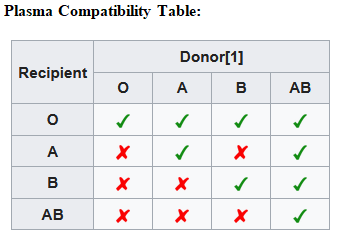
However, while AB blood type individuals can only donate blood to the same type, the reverse is true of plasma donations for them. This is because, again, AB individuals have neither A or B antibodies in their plasma. Thus, they are universal plasma donors.
On the other end of the spectrum, Type O , as noted, has neither A nor B antigens on its red blood cells, but both A and B antibodies in its plasma. As a result, those with type O- may donate to a person with every blood type, but can only receive O- blood since its plasma antibodies would attack anything else.
This is why, along with the fact that only 7% of humans are O-, those of the O- persuasion are highly encourage to donate blood often, first, potentially for themselves (which is particularly handy to do regardless of blood type if you know you have a major surgery coming up- this gets around any shortage issue, as well as gets around any of those aforementioned potential compatibility caveats.)
The second reason O- individuals are encouraged to donate often is, of course, because this can benefit most everyone. This is particularly the case when in an emergency there may not be time to figure out what blood type a person is and thus if O- is on hand, that can be reasonably safely used immediately if absolutely necessary.
If you’re wondering about the full list of main blood types blood and plasma compatibilities, we have these two charts where you’ll note they are more or less inverses of one another in terms of compatibilities between donor and recipient for reasons previously explained:


Moving on to white blood cells, there are 6 main types of white blood cells. They are: Neutrophils, Eosinophils, Basophils, Bands, Monocytes, and Lymphocytes. Each type plays a different role in the kind of infection your body is trying to fight. For example, Neutrophils kill bacteria by ingesting them (called phagocytosis). Naturally, if you have a bacterial infection, the percentage of neutrophils within your blood would be elevated.
On that note, in the general case, white blood cells number approximately 4-10 thousand per microliter of blood. If that number is increased, then you probably have an infection that your body is trying to fight and you are going to drop dead any… time… now…. Go ahead, we’ll wait…
As you might expect from this, when a doctor draws your blood to find out what’s wrong with you, it’s these levels of white blood cells that will help them narrow down the cause of your problem.
The last part of blood is the aforementioned plasma. This makes up most of your blood volume and about 90% of plasma is simply water, with another 8% of plasma made up of proteins, such as Albumin which helps move molecules like calcium and medications through your blood, antibodies that help with infection, and fibrinogen and clotting factors that help with the clotting of your blood.
The other 2% of plasma contains hormones like insulin, electrolytes like sodium and potassium, and nutrients like sugars and vitamins.
And one last little tip from the paramedic author of this particular piece- how to get blood stains out of clothes.
If you spill or otherwise get blood on your clothes when that special someone takes too long to die on his own, just soak it in 1 quart warm water, 2 teaspoons of laundry detergent and 1 tablespoon of ammonia for approximately 15 minutes. Then remove all the ammonia and launder it normally. (And note: don’t dry it until the stain is completely gone.) Bam! Your clothes will be blood free and the cops will never be able to link anyone’s death to you!
If you liked this article, you might also enjoy our new popular podcast, The BrainFood Show (iTunes, Spotify, Google Play Music, Feed), as well as:
Bonus Facts:
Speaking of blood, a commonly touted idea is that de-oxygenated blood turns blue. It turns out, however, this isn’t true at all. The misconception that blood that lacks oxygen turns blue probably comes from the fact that veins appear blue and blood in the veins is typically heading back to the lungs, hence depleted of oxygen. It is also possibly from the fact that when people are suffocating or the like, their lips and complexion seem to turn blue-ish or purple.
As to why veins often appear blue in those of the fairer skinned persuasion, this simply has to do with that they are very close to the surface of skin, combined with the way light diffuses in skin of certain shades. More specifically, veins may appear blue in some people from the way subcutaneous fat absorbs low-frequency light. This permits only high frequency blue and violet wavelengths to penetrate through the skin to the vein, with the other wavelengths getting filtered off from the pigmentation of your skin. In fact, when skin is removed, such as when dissecting a cadaver, or when you’re giving that special someone what they deserve, the veins and arteries actually are a somewhat similar color.
A similar light diffusion process is happening when we see people who are suffocating and have purple lips and fingertips. In this case, the blood is so oxygen deprived that it turns an extremely dark shade of red. When the light diffuses through the skin of the lips or through your fingernails, it then often ends up looking very dark blue or purple.
In reality of course, blood is various shades of red, with the red color primarily coming from the hemoglobin, which contains four heme groups. These heme group’s interactions with various molecules end up giving it the dark red or light red color we see, usually, with some caveats like with carbon monoxide poisoning, being lighter red when particularly oxygenated and darker red when it has less oxygen.
There are some creatures that have blue blood, for example horseshoe crabs, whose baby blue blood is actually worth around $60,000 per gallon… Why?
This is due to a chemical found in the amoebocytes of its blood. When this is exposed to a potentially dangerous foreign bacterium, it will immediately coagulate around the threat, rendering it harmless without actually destroying it. This effect is near instant and the blood can be used to detect a potential threat even if it’s diluted as much as one part in a trillion!
This effect is amazingly useful for detecting bacterial contamination in things like medicines and vaccines, or on medical equipment like needles, pacemakers, and numerous other items that are required to be sterile. In fact, no drug on the market today can be certified by the FDA unless it has been tested using this exact method (known as the Limulus amebocyte lysate test, in homage to the species of the crab- Limulus polyphemus). It’s by far the best way scientists are aware of for detecting whether a batch of medicine or vaccine has been compromised or not. As such, the blood of these crabs is worth a small fortune, selling for around $60,000 per gallon.
If you’re wondering how this blood is harvested, the crabs (over a half a million per year) are carefully picked up when they visit the shore for breeding purposes and taken in cooled trucks to certified labs where around 30% of their blood is drained, after which they’re returned to the sea. The blood cells are then separated using centrifugation. Next, the isolated cells are placed in distilled water where they will eventually burst, releasing the valuable chemical inside. After being purified, it is then freeze-dried and stored to be used for testing.
Approximately 85%-97% of the crabs harvested for this purpose survive and go on their merry way after, with the crab’s blood levels returning to normal in under a week.
Even with the relatively good survival rates, all of this may sound harsh. But there is one type of animal besides humans that, at the least, is glad this property of horseshoe crab blood was discovered in 1956 by Dr. Frederik Bang- namely, the rabbit. Before the horseshoe crab blood method (LAL) of detecting microbial contaminants, a much less accurate and time consuming system involving testing on live rabbits was used. (In this rabbit pyrogen test, the rabbits were injected with a sample of the substance to be tested.)






































 There are several different types of blood. Contained within them are different types of cells and countless molecules that give our bodies the needed nutrients to work effectively. The two main types of cells within the blood are red and white blood cells. Red blood cells make up nearly 45% of your blood volume. White blood cells make up less than 1%. What is left over is known as blood plasma, which makes up approximately 55% of your blood volume.
There are several different types of blood. Contained within them are different types of cells and countless molecules that give our bodies the needed nutrients to work effectively. The two main types of cells within the blood are red and white blood cells. Red blood cells make up nearly 45% of your blood volume. White blood cells make up less than 1%. What is left over is known as blood plasma, which makes up approximately 55% of your blood volume.